Cardiac Function Dataset
Description
This study was designed to assess if phonocardiogram (PCG), photoplethysmogram (PPG) and electrocardiogram (ECG) can be used to accurately measure systolic and diastolic time intervals as well as other parameters such as the stroke volume and cardiac contractility. The study was carried out with 68 volunteers in the “Centro Hospitalar da Universidade de Coimbra”, Coimbra, Portugal, which are divided into two distinct groups: one containing 33 healthy subjects and another with 35 subjects suffering from various cardiovascular diseases (CVDs), such as hypertension, arrhythmia, acute infarction, AV blocks (pacemaker), angina pectoris, heart failure, ischemia, aortic insufficiency, coronary artery disease and aortic stenosis.
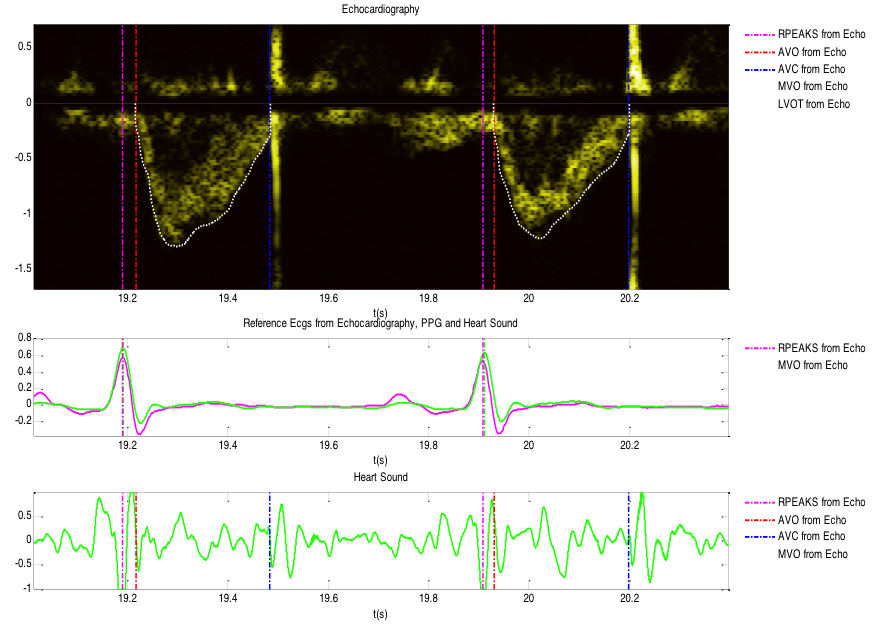
During this study, the volunteers were requested to stay at the supine position, at rest and after exercise (the healthy subjects), while the ECG (MLII lead configuration), PPG (right hand index finger), PCG (LSB – left sternum border, and apex) and echocardiography (Doppler mode) were collected by an authorized medical specialist. The measurement protocol consisted on the acquisition of echocardiographic data during several runs (at least 8 consecutive runs of 8 seconds), during which the remaining bio-signals were synchronously recorded.
Using the echocardiographic measurements, a clinical technician manually annotated several cardiac parameters, such as the pre-ejection period, the left ventricular ejection time, etc. and other parameters (such as stroke volume) were calculated based on the provided annotations. The population was not balanced for gender (51 male and 17 female). The biometric characteristics of the population are (mean ± std):
- Age: 29,72 ± 8,54 (Healthy subjects) and 58,97 ± 17,22 (CVD subjects) years
- BMI: 24,48 ± 2,41 (Healthy subjects) and 25,38 ± 3,10 (CVD subjects) Kg/m2
Possible use cases
The relevance of the main systolic time intervals is related to the fact that myocardial relaxation and contraction are governed by intracellular recycling of calcium ions. The timings of these basic cardiac events are directly related to the health of the cardiac cells and determine the ability of the myocardium to achieve blood delivery according to the metabolic requirements of the organs. Of major importance are the systolic and diastolic timings of the left ventricle, since it is this ventricle’s function to insure the blood flow in the systemic circulation. In the mid 20th century PEP was studied extensively as a measure of cardiac systolic function, whereas LVET was applied as a surrogate of left ventricle stroke volume. A healthy heart exhibits a short PEP and a long ejection time, while myocardial dysfunction prolongs PEP and shortens LVET. This has led to the introduction of the PEP/LVET index to assess the systolic function of the heart. Indeed, a good and significant correlation between PEP/LVET and the left ventricle ejection fraction determined using angiography has been observed among patients with a wide variety of cardiovascular diseases. Furthermore, it was found that in patients with coronary artery disease, the PEP/LVET ratio is a highly reproducible measure that is equivalent in accuracy to the determination of the left ventricle ejection fraction. Despite the introduction of powerful and complete assessment tools of cardiac function such as the echocardiography, a significant interest in STI as a non-invasive tool for left ventricle function assessment persists in several contexts where portable, low intrusive and cheap solutions are imperative, such as in pHealth.
Parameters
The parameters available in the data set, collected in a daily basis, are:
Time series:
- ECG – runs between ap. 8s (from ECHO) and 400s (from HP monitor)
- PPG – runs of ap. 400s
- PCG – runs of ap. 30s
- Echocardiography – ap. 8 runs of 8 secs
Meta data:
- Weight
- Height
- Body mass index
- Age
- Gender
- Cardiovascular disease/condition
Annotations
Based on the echocardiographic images a clinical technician annotated several hemodynamic measures, which are listed below:
- ECG R-peaks – Beat-to-beat
- Aortic valve opening (AVO) – Beat-to-beat
- Aortic valve closure (AVC) – Beat-to-beat
- Mitral valve opening (MVO) – Beat-to-beat
- Heart Rate (HR) – Beat-to-beat
- Pre-ejection Period (PEP) – Beat-to-beat
- Left ventricular ejection time (LVET) – Beat-to-beat
- Isovolumetric relaxation time (IRT) – Beat-to-beat
- Left ventricular outflow tract (LVOT) diameter – Average (onset of the protocol)
- Left ventricular outflow tract (LVOT) trace – Curve/beat-to-beat
- Left ventricular outflow tract (LVOT) velocity time integral (VTI) – Beat-to-beat
- Stroke volume (SV) – Beat-to-beat estimation from LVOT diameter and VTI beat-to-beat
- Cardiac output (CO) – Calculated beat-to-beat
- Ejection Fraction – Average (onset of the protocol)
Access:
This database is available to logged users using the link below.
How to cite this database:
P. Carvalho and Paiva, R.P. and Henriques, J. and Antunes, M. , “Assessing Systolic Time-Intervals from Heart Sound: a Feasibility Study”, in EMBC-2009, 31st Annual International Conference of the IEEE Engineering in Medicine and Biology Society, 2009
Contact us
This dataset was used in the support of:
ICBHI 2019 Scientific Challenge
